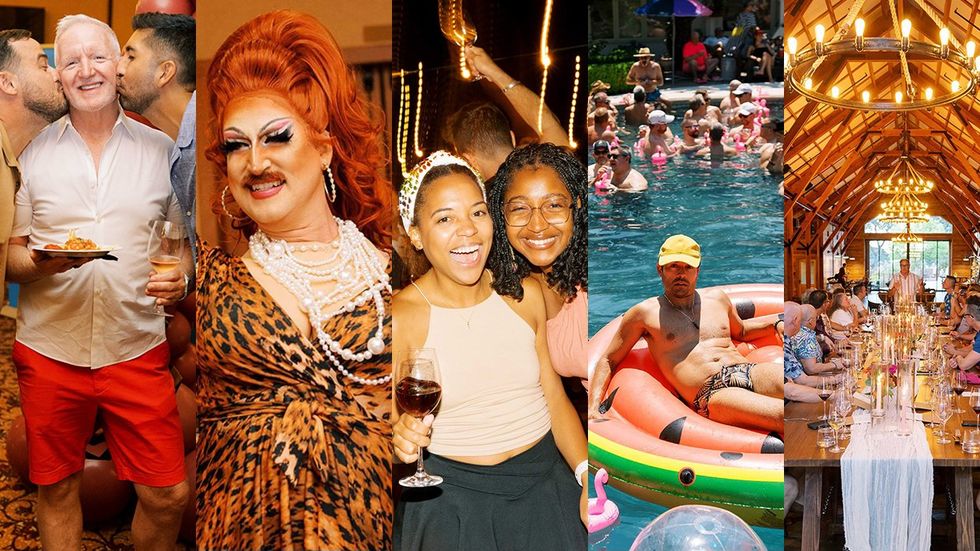
HIV testing doesn’t need to take place in a dingy clinic. It’s inconvenient, inaccessible, and still highly stigmatized for many men and women. HIV testing should be brought to the people. That’s the philosophy of the University of California, San Francisco, Alliance Health Project. HIV test counselors and phlebotomists drive around San Francisco in a van that boldly states "FREE HIV TEST" on the side, offering free screenings to all who want them. Results come back in just 20 minutes, so the client doesn’t need to call in.
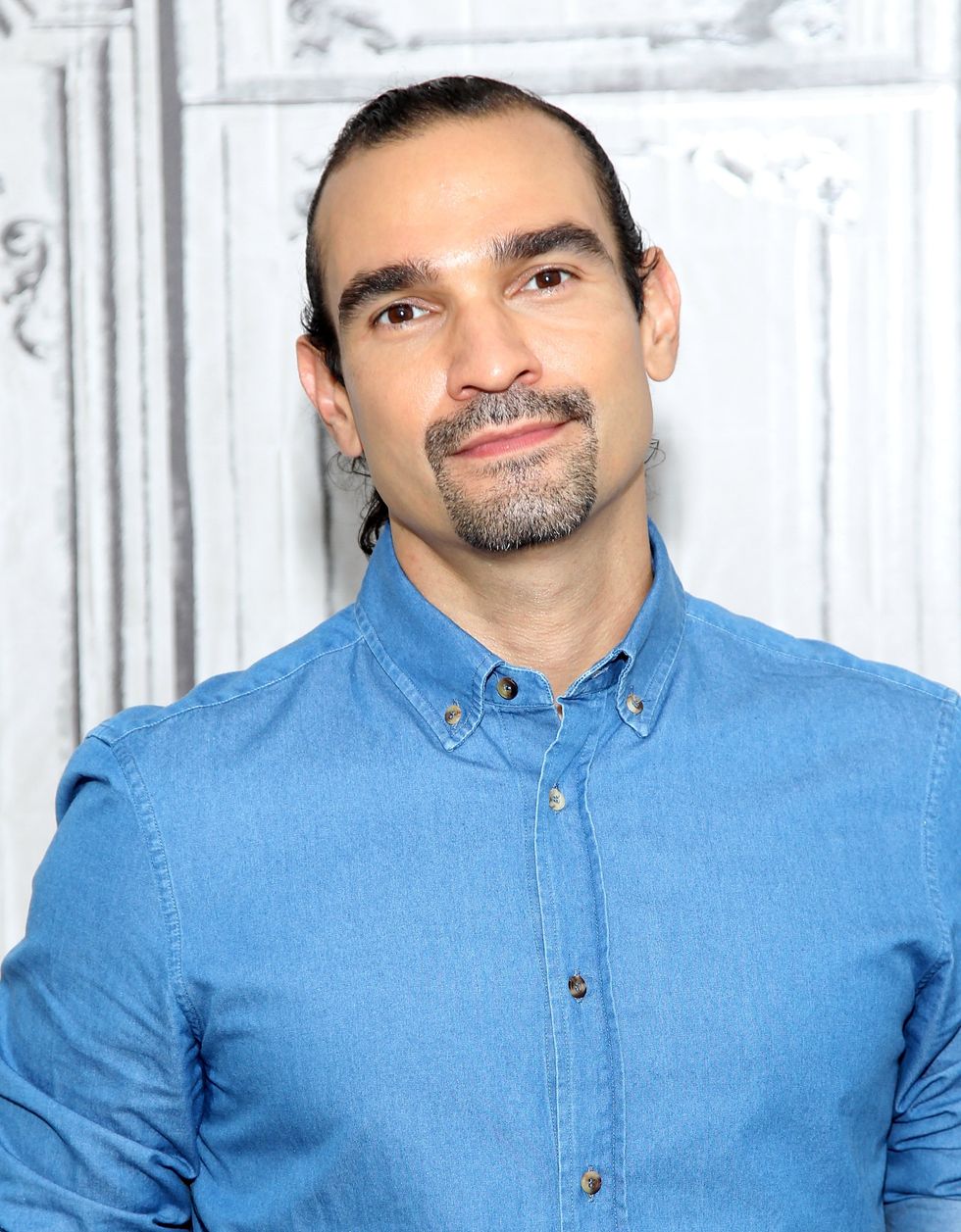
Brandi Ly, a mobile HIV test counselor who’s been working for the UCSF Alliance Health Project for over two years, shared some of her knowledge with Pride in an exclusive interview. Here are eight things we learned from her.
“You learn it’s not the end of the world. You’re already infected. There’s nothing you can do to reverse that. Providing clients the knowledge that they are infected and the steps they can take to improve their health is our goal. And by telling them what they can do, we really hope to empower them.”
“A lot of hugs are given. And some people cry. They cry when they’re told they’re preliminarily positive and negative. More often than not, people have a sense that they’re already HIV-positive, and the test is just confirming what they think. But there are sometimes it comes as a complete shock to them.”
“San Francisco’s model is test to treat. Our job is to link up with that person and figure out what the best next steps are, and hopefully that’s treatment.” Brandi also mentioned that pushing treatment is not necessarily productive if the patient isn’t ready. She discussed how it’s necessary as a counselor to meet patients where they’re at.
“[There is] such a divide among opinions of older and younger generations of gay men. ... Older gay men have been conditioned to always wear condoms. They remember what it’s like when their friends died back in the ’80s ... and they often feel shame and guilt when they don’t [use a condom]. Younger gay men often don’t have the same guilt or fear of not wearing condoms.”
Brandi mentioned that there are plenty of factors that could be contributing to the rise of chlamydia, gonorrhea, and syphilis in the LGBT community in San Francisco. While no one knows exactly why rates have started to increase, she mainly attributes the rise to the increased use of hookup apps. She also mentioned that this rise may be due to pre-exposure prophylaxis (PrEP). More men are taking Truvada as PrEP to prevent HIV and are no longer using condoms. While Brandi mentioned that PrEP does drastically decrease the chances of acquiring HIV, it should still be used with condoms to increase efficacy (and to prevent spreading of other STDs).
“Despite being one of the highest populations at risk for HIV, HIV has decreased among the injection drug user community in San Francisco. Some studies accredit the lower rates of HIV among intravenous drug users to the needle exchange programs in S.F.” While needle exchange is not one of the UCSF Alliance Health Project’s services (although leaders there are hoping to start one soon), the project still does test for hepatitis C in its van. Hep C greatly affects injection drug users, and many people with HIV also have hep C.
The UCSF Alliance Health Project is one of the few mobile testing services to use fourth-generation HIV rapid tests. The fourth-generation HIV test screens for both HIV antibodies and the p24 antigen. Antigens are detectable before antibodies, so by screening for both, this test cuts down the window period during which your HIV status cannot be determined conclusively. You’re most infectious during acute infection, which occurs shortly after exposure. During this time, your viral load spikes before your immune system can help to control it. It’s in this period you are most likely to spread HIV. Using the fourth-generation rapid test, the mobile testing can catch infection during the first few weeks.
The key is getting into treatment to lower your viral load. If your viral load is undetectable, it is less likely you will pass on HIV to your partner. There are also additional steps to protect yourself and your partner, such as PrEP. And of course, condoms. As Brandi repeatedly emphasized, “HIV is not a death sentence,” and there have been great advances in treatment in the past 15 years. People who are infected with HIV live nearly 20 years longer on average than they did in 2001.
Want to learn more about the UCSF Alliance Health Project?
UCSF Alliance Health Project home page
HIV Testing and Counseling Program
Facebook